Managing Diabetes in the Summer Heat: A Guide for Patients

As the monsoon season ends and the full heat of summer begins, individuals with diabetes face challenges beyond just the heat. Rising temperatures lead to increased sweating, decreased appetite, and reduced physical activity.
These combined changes can make blood sugar control more difficult during the summer months.
Why is blood sugar control challenging in the summer, and how can you manage your blood sugar levels while staying cool?
This post will cover the causes of blood sugar fluctuations in diabetic patients during the hot summer and provide management tips for a safe summer.
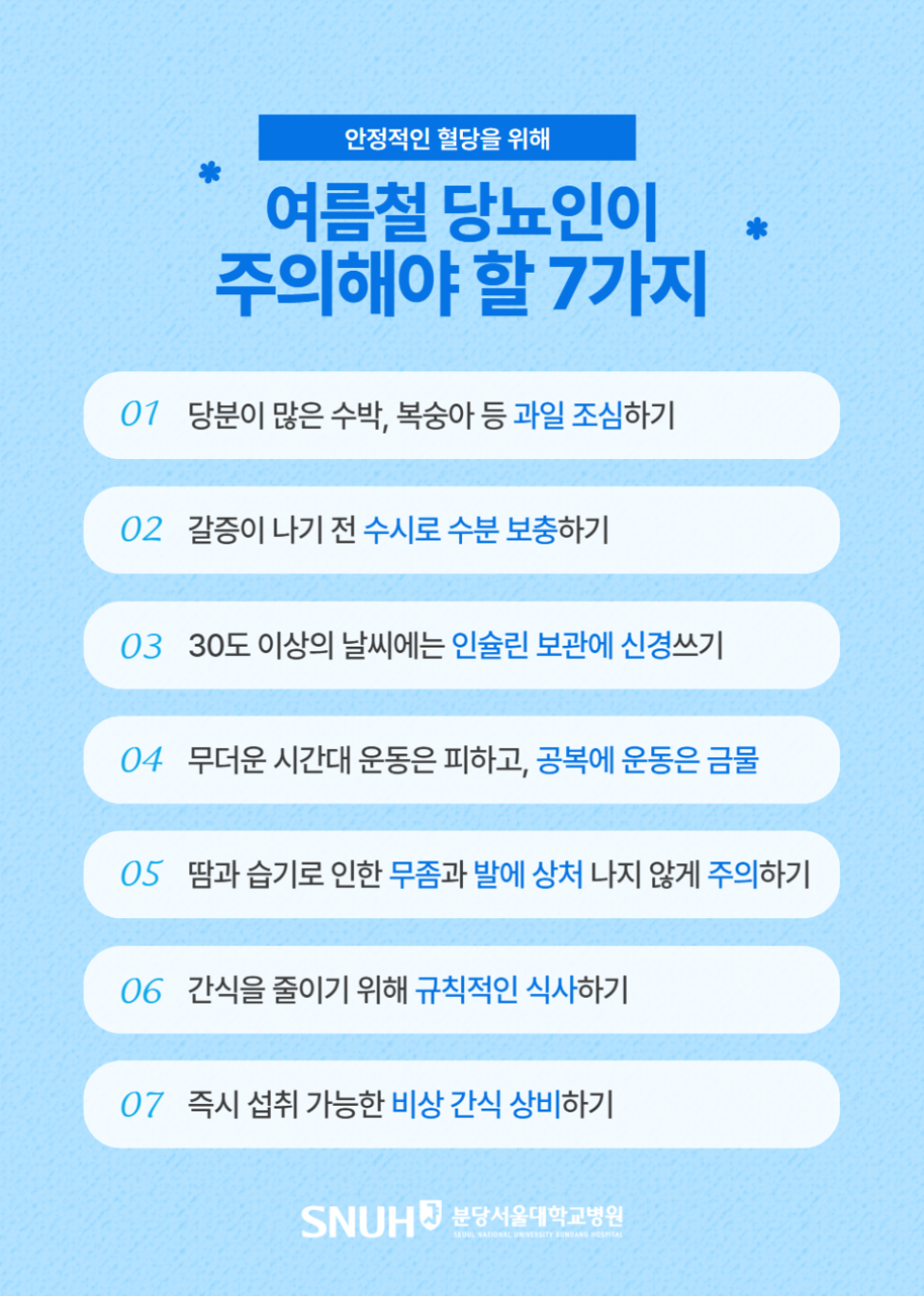
7 Important Precautions for Diabetics in the Summer
1. Be Careful with Summer Fruits
Fruits like watermelon, Korean melon, and peaches, which are commonly consumed in summer, are refreshing due to their high water content but can rapidly raise blood sugar levels due to their high sugar content. Juices made by blending these fruits with added sugar can cause an even faster spike in blood sugar.
2. Stay Hydrated
Excessive sweating due to the heat can lead to dehydration, which can concentrate the blood and increase blood sugar levels. It's important to drink water or electrolyte beverages frequently, even before you feel thirsty.
3. Insulin Storage Temperature
Insulin is sensitive to heat and can degrade or become ineffective if not stored properly. Refrigerate insulin if the room temperature exceeds 30 degrees Celsius. When engaging in outdoor activities, use a cooler or insulated pouch to maintain the appropriate temperature, especially inside vehicles.
4. Adjust Exercise Intensity and Timing
Avoid strenuous exercise during the hottest part of the day. Opt for light exercise in the early morning or late evening. It is better to exercise 30 minutes to 1 hour after a meal rather than on an empty stomach for better blood sugar control. Avoid intense exercise on an empty stomach, and bring water and a light snack.
5. Foot Care
Sweat and humidity in the summer increase the risk of athlete's foot or foot injuries. Because diabetic patients heal slowly, even minor injuries can lead to infection if neglected. Wash and dry your feet thoroughly daily, and be cautious to avoid foot injuries during water activities.
6. Regular Meals
High temperatures can reduce appetite, leading to irregular meal times or increased consumption of sugary drinks like soda, coffee, juice, or ice cream. Maintaining regular meal times and monitoring blood sugar levels after meals are crucial for blood sugar control during the summer.
7. Carry Emergency Snacks
When traveling long distances or exercising, blood sugar levels can drop rapidly. Carry easily portable, individually packaged snacks. Keep glucose tablets, candies, or juice readily available in your bag, car, or pocket to quickly address suspected hypoglycemia.
Why Summer is More Difficult for Diabetics: Hyperglycemia and Dehydration
In the summer, excessive sweating due to hot weather can lead to rapid dehydration, concentrating the blood and raising blood sugar levels. Waiting until you feel thirsty to drink water may be too late. Make it a habit to drink small amounts of water frequently, even when not thirsty. Severe dehydration can make blood sugar control more difficult and, in severe cases, lead to emergencies like diabetic ketoacidosis.
Diabetic patients may have impaired thermoregulation due to peripheral blood vessel or autonomic nervous system damage, increasing the risk of heatstroke. Avoid going out or engaging in outdoor activities during the hottest part of the day, take frequent breaks in cool places, and regulate your body temperature.
Why is Low Blood Sugar (Hypoglycemia) Dangerous?
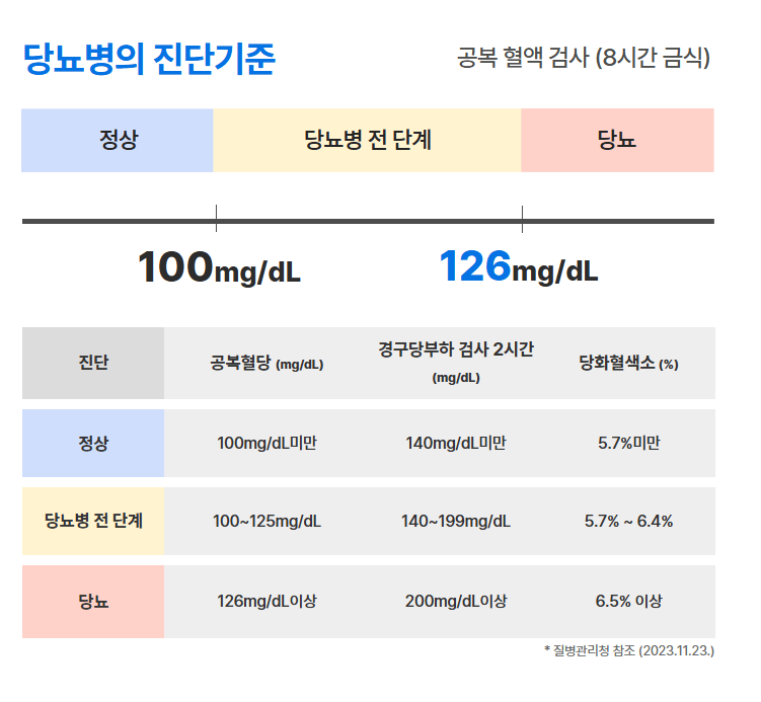
Hypoglycemia refers to a condition where blood glucose levels become too low. Generally, hypoglycemia is diagnosed when blood sugar levels drop below 70mg/dL, and levels below 54mg/dL are considered severe hypoglycemia.
In most cases, there are few or no symptoms when blood sugar levels are around 70mg/dL. However, individual sensitivity varies, and some people may experience symptoms of hypoglycemia even at levels above 70mg/dL.
Symptoms of hypoglycemia can include sudden trembling, extreme hunger, cold sweats, palpitations, and dizziness. If left untreated, it can lead to neurological symptoms such as confusion, slurred speech, and blurred vision, and in severe cases, it can progress to emergencies like fainting or seizures.
Nocturnal hypoglycemia, which occurs during sleep, is particularly dangerous because it can worsen unnoticed. Repeated episodes of hypoglycemia can cause some patients to avoid lowering their blood sugar levels due to fear, which can increase the risk of long-term complications.
Hypoglycemia is dangerous not only because of the abnormally low blood sugar itself but also because it can lead to unexpected hyperglycemia.
When blood sugar levels drop below 70mg/dL overnight, the body releases hormones like glucagon, cortisol, and adrenaline to raise blood sugar levels. This can result in the Somogyi effect, where morning blood sugar levels are higher than usual.
The problem is that this phenomenon can be mistaken for simple hyperglycemia. Increasing medication dosages without accurately identifying the cause can worsen the situation. In reality, if hypoglycemia occurred in the evening or early morning, reducing medication or adjusting the timing may be appropriate. Additionally, if eating before bed causes elevated blood sugar levels to persist throughout the night, dietary adjustments should be prioritized over medication adjustments.
Managing diabetes in the summer can be challenging, but taking a little extra care to maintain stable blood sugar levels can greatly contribute to your health. Pay attention to small changes in your body, and do not hesitate to consult with a healthcare professional if you suspect symptoms of hypoglycemia or hyperglycemia.
Moon Jun-ho, Professor of Endocrinology and Metabolism
More helpful information from Bundang Seoul National University Hospital
View other posts







Source :https://blog.naver.com/happy_snubh/223958576490
No comments yet.
