Vitiligo: Causes, Management, and Treatment Options

Vitiligo is an autoimmune skin disorder characterized by the destruction of melanocytes, leading to the loss of pigment in certain areas of the skin, causing them to turn white. Recently, the condition garnered significant attention after Korean celebrity, Kian84, revealed his diagnosis on the popular TV show 'I Live Alone'.
So, what exactly is vitiligo, and how should it be managed and treated?
Let's delve into the causes of vitiligo, differentiate it from other skin conditions with similar symptoms, and explore everyday management techniques with Professor Choi Jong-won from the Department of Dermatology.
Vitiligo cases are steadily increasing in South Korea. According to data from the Health Insurance Review and Assessment Service, the number of patients seeking treatment for vitiligo has been on the rise. From 49,561 patients in 2010, the figure reached 65,460 in 2019, marking a long-term increase of over 32%. The current statistics only reflect the number of 'patients who received treatment,' and the actual number of vitiligo patients in Korea is estimated to be higher.
Why does vitiligo occur?
Vitiligo is an autoimmune disorder in which the immune system mistakenly attacks and destroys melanocytes, the cells responsible for producing melanin, the pigment that gives skin its color. Normally, the immune system protects the body from foreign substances like viruses and bacteria. However, in autoimmune diseases, the immune system malfunctions and cannot distinguish between body tissues and foreign invaders, leading it to attack the body's own cells and tissues.
As melanocytes are destroyed, they can no longer produce melanin, which determines skin and hair color. This leads to gradual depigmentation and the appearance of white patches on the skin.
These white patches are characterized by their distinct borders and irregular shapes, gradually spreading across the skin. They can appear anywhere on the body, especially on commonly exposed areas like the face, hands, and feet. The appearance of these patches on visible areas can cause significant mental and psychological distress for patients.
As the condition progresses, the patches may expand, and if the melanocytes in hair follicles are also destroyed, it can lead to leukotrichia, where the hair within the patches turns white. Aside from the skin patches, vitiligo is not typically associated with itching or pain, and it is not contagious.
The rate of progression varies from person to person. Early treatment is associated with better outcomes, so it is recommended to seek prompt diagnosis and treatment upon noticing white patches. Furthermore, due to the possibility of recurrence even after treatment, continuous monitoring and timely intervention are advised.
The exact cause of vitiligo is not yet fully understood. Current research suggests that it arises from a combination of factors, including genetic predisposition, antioxidant deficiencies in the autoimmune system, trauma such as sunburns, congenital melanin deficiencies, and psychological stress.
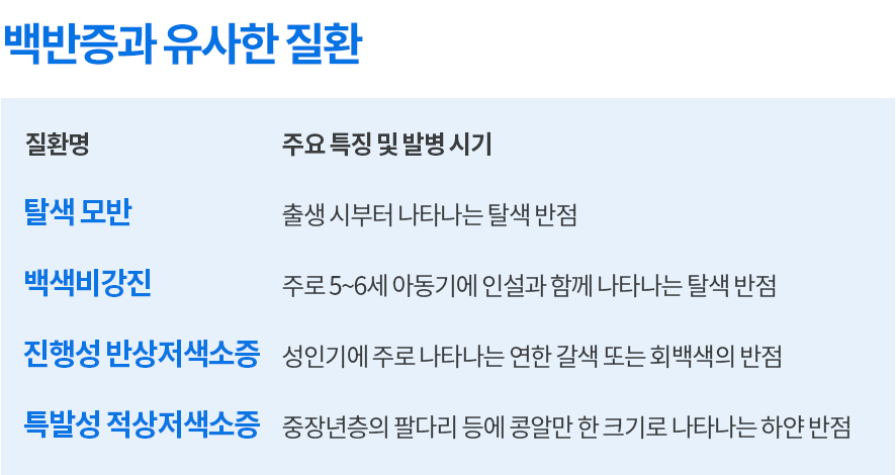
Conditions that can be mistaken for vitiligo
Several conditions can cause white spots on the body, not just vitiligo.
Common conditions that may present with white spots include nevus depigmentosus at birth, pityriasis alba in children aged 5-6, progressive macular hypomelanosis in adults, and idiopathic guttate hypomelanosis, characterized by small, coin-sized white spots in middle-aged and older adults.
Given the variety of skin conditions that can cause white spots, it is essential to consult a specialist for accurate diagnosis.
Vitiligo Treatment Methods
Vitiligo treatment primarily involves medication, phototherapy, and surgical options.
Medications, such as corticosteroids or topical immunomodulators, are used to control the autoimmune response and protect melanocytes from destruction. However, long-term use of corticosteroids can pose risks to blood pressure and joints, so they are typically prescribed for short periods of 4 to 8 weeks. Topical immunomodulators with minimal side effects are now more commonly used.
Phototherapy involves exposing the white patches to ultraviolet (UV) light to stimulate melanocytes around the patches, encouraging them to migrate and repopulate the affected areas. Phototherapy can be administered as whole-body irradiation or as localized treatment, depending on the size of the vitiligo patches.
A typical course involves at least 20 phototherapy sessions over 6 to 12 months. Patients may notice a gradual reduction in patch size within a couple of months of treatment. While the treatment requires long-term commitment and may involve periods of paused treatment if ineffective, adherence to a specialist's guidance can lead to significant improvement.
For areas that are difficult to treat, surgical procedures involving the transplantation of melanocytes from healthy skin tissue may be considered. However, as the transplanted skin may differ from the surrounding skin and the procedure does not eliminate the underlying condition, it is generally reserved as a last resort.
Vitiligo, like diabetes or rheumatoid arthritis, is often difficult to cure completely. However, with proper medical care and management, the condition can be significantly improved. Early diagnosis and treatment are associated with better outcomes, so seeking prompt medical evaluation is highly recommended.
Prevention and Management of Vitiligo
Firstly, avoid strong sunlight. Ultraviolet (UV) radiation is a major factor in triggering and exacerbating vitiligo. Without melanocytes, the skin is prone to sunburn, increasing the risk of worsening vitiligo. UV radiation can also cause skin cancer. Even UV therapy requires rest periods due to its potential risks. The intensity of UV exposure should be carefully managed and monitored in consultation with a healthcare professional.
Applying sunscreen is crucial to protect the skin from UV rays. While sunscreen is recommended for everyone to protect their skin, it is especially important for those with vitiligo or a history of skin conditions, particularly when exposed to sunlight.
Secondly, avoid inflammation from trauma. Inflammation caused by injuries can trigger the body's immune system, leading to increased attacks on melanocytes. Special care should be taken to avoid irritating the scalp with hair dyes.
Thirdly, maintain a healthy lifestyle. Vitiligo involves the destruction of melanocytes, and a healthy body is essential for their regeneration. Adequate sleep, exercise, and avoiding alcohol, smoking, and inflammatory foods are important.
Consuming antioxidant-rich vitamins, such as vitamins A, C, and E, through vegetables or supplements is recommended. However, it is important to remember that no specific food or nutrient can cure vitiligo. Dietary and lifestyle management should be viewed as a means to maintain overall health.
Vitiligo is a chronic condition where early diagnosis, specialized care, and consistent treatment can significantly improve symptoms.
Do not be discouraged, and work with a dermatologist to develop a specialized treatment plan.
Professor Choi Jong-won, Department of Dermatology
More helpful content from Bundang Seoul National University Hospital
View other posts









Source :https://blog.naver.com/happy_snubh/224047406483
No comments yet.
